Flatback Syndrome
Flatback Syndrome
 When the proper curves in the spine that support an economical stance requiring minimum energy to stand or walk fail, the result is a condition called Flatback syndrome.
When the proper curves in the spine that support an economical stance requiring minimum energy to stand or walk fail, the result is a condition called Flatback syndrome.
Some of the symptoms include having trouble maintaining a proper posture, low back pain and thigh pain. Since the person has trouble maintaining proper alignment, the symptoms might increase throughout the day due to fatigue. Patients might also have upper back and neck pain due to constantly trying to realign themselves. These symptoms can often develop to be very painful and disabling.
Flatback syndrome might be from a previously operated scoliosis. Flatback syndrome was originally used to describe Harrington rods recipients (1960s- early 1990s) due to the fact the rods sometimes flattened the normal sway of the spine. This was due to the rods extending down into the lower part of the spine. The rods were unable to follow the natural curve of the lower back, which caused the spine to unnaturally straighten out. This unnatural movement helped advance the degeneration of discs in the spine.
However, flatback syndrome with severe stooping might be from back ageing, osteoporosis, degenerative disease, lumbar surgery that fails.
No matter the cause, this can manifest as progressive stooping, which can cause severe pain and disablity.
If conservative treatment fails, surgery has dramatic results in standing patients up straight, relieving pain, and improving function.
Case Study
Flatback from Harrington Rods

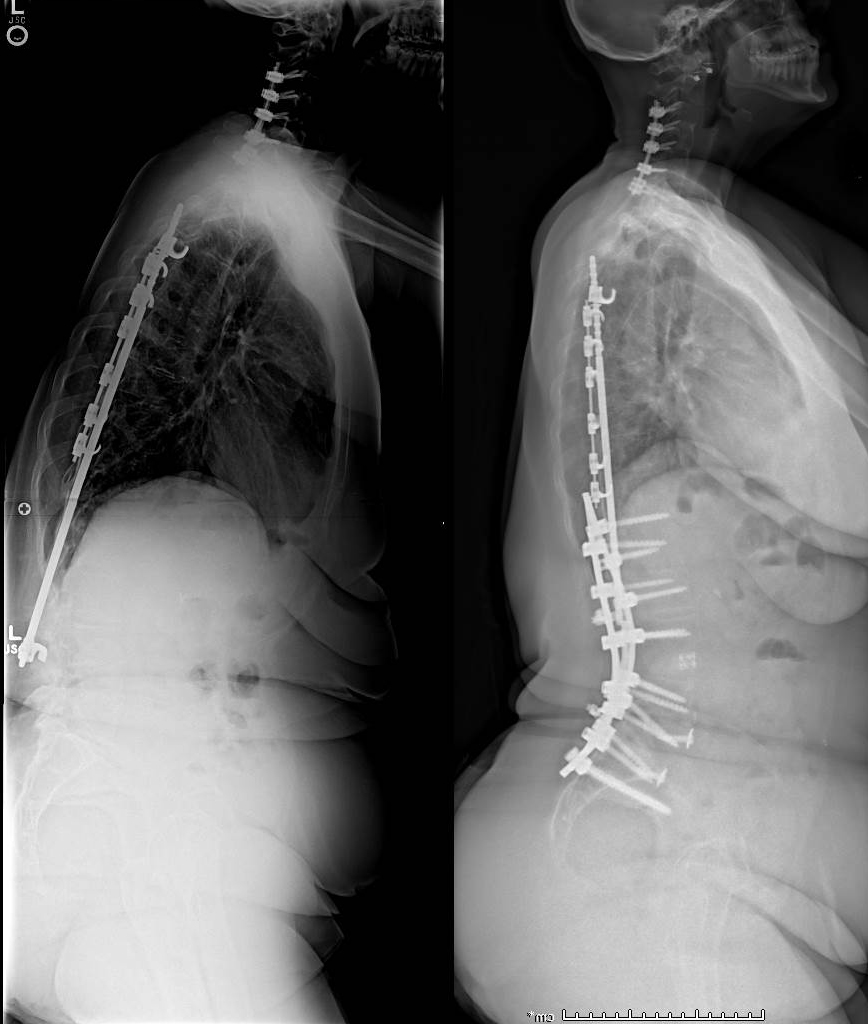 This 66 year old woman had a scoliosis fixed with CD rods when she was a teenager. She noticed over the previous 20 years progressive stooping forward, and severe physical pain and cosmetic deformity. She performed 6 weeks of Physical Therapy with our Spine Specialized physical therapist with no avail. Her diagnosis was severe flatback from lumbar kyphosis and thoracolumbar kyphosis. She was given a nutritional plan and a medical clearance, and in 2016 we performed a T3-Pelvis complex spinal reconstruction with posterior column osteotomies at T7-L1, and a 3 column Type 4 pedicle subtraction osteotomy at L4. 6 weeks later she had a 1.5 hour mini open anterior lumbar inter body fusion at L5S1 to additionally fuse this level.
This 66 year old woman had a scoliosis fixed with CD rods when she was a teenager. She noticed over the previous 20 years progressive stooping forward, and severe physical pain and cosmetic deformity. She performed 6 weeks of Physical Therapy with our Spine Specialized physical therapist with no avail. Her diagnosis was severe flatback from lumbar kyphosis and thoracolumbar kyphosis. She was given a nutritional plan and a medical clearance, and in 2016 we performed a T3-Pelvis complex spinal reconstruction with posterior column osteotomies at T7-L1, and a 3 column Type 4 pedicle subtraction osteotomy at L4. 6 weeks later she had a 1.5 hour mini open anterior lumbar inter body fusion at L5S1 to additionally fuse this level.
2 years later, she can walk over 2 miles, rates her pain level as none, and her disability level as zero (VAS 0, ODI 0). She participates in fitness classes and a walking program, and lives independently alone.