Kyphosis Overview | Adolescent Kyphosis | Adult Kyphosis | Dengerative Scoliosis | Adolescent Scoliosis | Adult Scoliosis | Flatback Syndrome | Harrington Rod | Idiopathic Scoliosis | Lordosis | Previously Operated Scoliosis | Other Types
 Overview
Overview
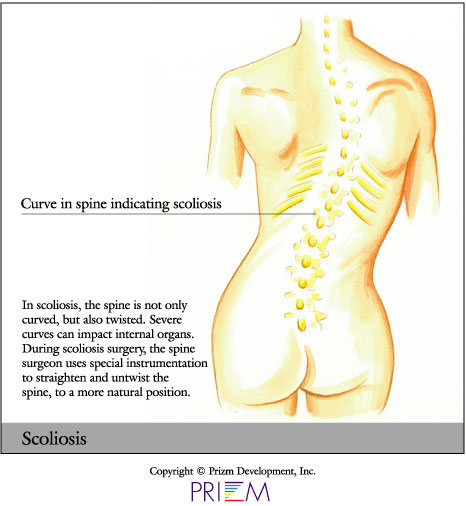 Scoliosis is an abnormal curvature of the spine in the coronal plane (facing the patient or their back head on) of more than 10 degrees. Often the most common kinds of scoliosis can first appear during childhood. Some people are born with it, while others develop it over time. Scoliosis can cause the spine to twist and bend in an abnormal way. The cause of scoliosis is unknown, but it is genetic, and it does tend to affect more women than men.
Scoliosis is an abnormal curvature of the spine in the coronal plane (facing the patient or their back head on) of more than 10 degrees. Often the most common kinds of scoliosis can first appear during childhood. Some people are born with it, while others develop it over time. Scoliosis can cause the spine to twist and bend in an abnormal way. The cause of scoliosis is unknown, but it is genetic, and it does tend to affect more women than men.
It is very important to individually assess cases of scoliosis. Sometimes a back brace is used to prevent worsening of the spine curvature. Adolescent scoliosis can progress even after skeletal maturity, if the curvature is larger than 40 degrees in the thoracic spine or larger than 30 degrees in the lumbar spine, the scoliosis should be monitored about every 5 years if no symptoms are present.
Dramatic curves of the spine can place pressure on internal organs. If this happens, surgery may be necessary. If left untreated, severe cases of scoliosis can shorten a person's life span.
In less severe cases, scoliosis may cause the bones to twist slightly, making the hips or ribs appear uneven. When this occurs, the problem is more an issue of pain and deformity and less of a health risk.
Scoliosis surgery is complex, and a person should invest a great deal of time in choosing an orthopedic surgeon who uses the most current surgical techniques, implants, and bone graft substitutes. Surgeon experience and specialization have direct effects on eventual cosmesis, patient outcome and results, and both deformity correction and patient reported outcome scores (PRO) and Health Related Quality of Life (HRQRL)
[Top]
Causes
Scoliosis can be caused by a genetic growth disturbance (previous unknown, such as Adolescent Idiopathic Scoliosis), from a formation or segmentation defect of a vertebra or many vertebrae (Congenital Scoliosis), a neuromuscular condition (such as Myelodysplasia or Cerebral Palsy), or from a syndrome, tumor, fracture or poorly done spinal operation.
Your care provider can discuss more the cause of your scoliosis and how that impacts potential treatments.
[Top]
Signs & Symptoms
Sometimes, scoliosis is visible. For instance, the patient may have uneven shoulders, chest, hips, shoulder blades, waist, or a child may have a tendency to lean to one side. In other cases, there are no visible signs. The severity of the scoliosis, the location, and the cause can be related to the physical signs.
Scoliosis can be noticed by a family member, pediatrician, family physician, or school screening. To diagnose a child with scoliosis, have them touch their toes. If either one or both shoulder blades are prominent, the waist is shifted or ribs are uneven, scoliosis may be present. For a child or teenager, your pediatrician often screens for scoliosis. There are school screening programs as well. [Top]
Diagnosis
Outlined below are some of the diagnostic tools that your physician may use to gain insight into your condition and determine the best treatment plan for your condition.
- Medical history: Conducting a detailed medical history helps the doctor better understand the possible causes of your back and neck pain which can help outline the most appropriate treatment.
- Physical exam: During the physical exam, your physician will try to pinpoint the source of pain. Simple tests for flexibility and muscle strength may also be conducted.
- X-rays are usually the first step in diagnostic testing methods. X-rays show bones and the space between bones. They are of limited value, however, since they do not show muscles and ligaments.
- MRI (magnetic resonance imaging) uses a magnetic field and radio waves to generate highly detailed pictures of the inside of your body. Since X-rays only show bones, MRIs are needed to visualize soft tissues like discs in the spine. This type of imaging is very safe and usually pain-free.
- CT scan/myelogram: A CT scan is similar to an MRI in that it provides diagnostic information about the internal structures of the spine. A myelogram is used to diagnose a bulging disc, tumor, or changes in the bones surrounding the spinal cord or nerves. A local anesthetic is injected into the low back to numb the area. A lumbar puncture (spinal tap) is then performed. A dye is injected into the spinal canal to reveal where problems lie.
- Electrodiagnostics: Electrical testing of the nerves and spinal cord may be performed as part of a diagnostic workup. These tests, called electromyography (EMG) or somato sensory evoked potentials (SSEP), assist your doctor in understanding how your nerves or spinal cord are affected by your condition.
- Bone scan: Bone imaging is used to detect infection, malignancy, fractures and arthritis in any part of the skeleton. Bone scans are also used for finding lesions for biopsy or excision.
- Injections: Pain-relieving injections can relieve back pain and give the physician important information about your problem, as well as provide a bridge therapy.
Treatment
There are roughly three tiers of treatment for scoliosis. These consist of observation, bracing, and surgery. In some cases, there are other options. The goal is to keep the curve from progressing to the point that there is deformity, pain, loss of function, or impacts on internal organs. In children and adolescents, the emphasis is on conservative treatments and the natural history of the disease process. For adults, the emphasis is on function, pain, and movement.
Surgery options including tethering, stapling, minimally invasive and open, and in the most severe cases, spinal osteotomy, may be required in order to correct the spinal curve. Surgery is usually only recommended for large, progressive curves or in those patients who have pain that steadily worsens.
[Top]
 Idiopathic Scoliosis
Idiopathic Scoliosis
Idiopathic scoliosis is the most common type of scoliosis, with onset after 10 (Adolescent Idiopathic Scoliosis) being the most common. For the other types of idiopathic scoliosis, when scoliosis is present before the age of 3, this is known as Infantile Scoliosis. When scoliosis is diagnosed between the ages of 3 to 10, this is known as Juvenile Scoliosis.
All Idiopathic Scoliosis seems to be a genetic growth disturbance. Depending on the age of the patient and the size of the curve, the patient may do best with observation, bracing, casting, growth sparing procedures such as grow rods, MAGEC, VEPTR, Shilla, tetherings or with reconstructive scoliosis correction and fusion, either minimally invasive or open.
It is important to involve a fellowship-trained physician that specializes in scoliosis scoliosis and spinal deformities. Surgeon experience plays a big role in patient outcome.
Click here to learn more about Idiopathic Scoliosis.
Adolescent Scoliosis
Early Onset Scoliosis (Birth to 7 years old)
Small children, from birth to 7 years of age, pose special challenges in the treatment of their scoliosis. In these patients, growth of the spine and the lungs via the ribcage are intertwined, and must be maintained. Causes can be infantile or juvenile idiopathic scoliosis, congenital scoliosis and rib fusions, or neuromuscular or genetic syndromes, or connective tissue disorders.
In these patients, initial attempts to control the scoliosis and maintain ribcage and lung growth can focus on observation, bracing, or casting, though one downside of bracing and casting is that braces and casts push on the ribcage as it grows. If this is not successful in progressive curves, then a variety of growth preserving procedures can be attempted, including growing rods, Shilla procedures, titanium rib or vertical expandable prosthetic titanium rib (VEPTR), MAGEC rod, or a stapling or tethering procedure. However, as their name implies, these growth preserving procedures may need multiple repeat surgeries to maintain growth, but this sometimes is the only way to maintain thoracic growth and lung function.
Older children
For patients 8 to 10 years old, again curves are observed unless large or progressing. Again, priority is given to preserving spine and rib cage growth. However, some patients may benefit from bracing, grow constructs, vertebral body stapling, minimally invasive reconstruction, or, rarely, open reconstruction. A simple genetics test using saliva (see Genetics Test for Scoliosis) may help your physician decide the best treatment for your child.
Adolescents
For patients 9 and older, again observation is the rule. If your child is 9-13 years old, they may be a candidate for the genetics test for scoliosis (see Genetics Test for Scoliosis), which may help avoid treatment your child does not need, or in cases in which the test predicts a severe curve, move to innovative, less invasive treatments to avoid open spinal reconstruction. Occasionally bracing may be of benefit. In these cases, the Boston Brace is used for thoracic and double curves, and the Charleston Brace can be used initially for lumbar located curves.
In patients with significant growth potential (8-12 skeletal age) with progressing curves, a high genetics test score, and curves 20-40 degrees, may benefit from vertebral body stapling, in which minimally invasive approaches are used to deliver a nitinol staple (see Vertebral Body Stapling). This procedure uses the spine's remaining growth to correct the scoliosis.
In large curves, over 40 degrees for lumbar curves and over 45 degrees for thoracic curves, surgery may be indicated. Preference is given to minimally invasive scoliosis reconstruction (see Minimally Invasive Approaches) when advisable.
 Stephanie - Adolescent Scoliosis |
 Rachel - Adolescent Scoliosis |
Young Adults
Skeletal maturity was once used as the benchmark for ending the treatment of idiopathic scoliosis. However, it is now recognized that curves over 30 degrees in the lumbar spine and 40 degrees in the thoracic spine have continued potential for progression. This progression can lead to worsening spinal deformity, pain, and accelerated degeneration of the spine around the scoliosis in the young adult.
Conservative treatments such as physical therapy and injections can often help with the pain issues. An opportunity may exist for a minimally invasive surgery addressing the scoliosis, which can correct the scoliosis, prevent further progression, and thus preventing degeneration of the spine below the scoliosis. This can prevent further pain and disability, and thus a larger, salvage surgery or progressive disability later in life.
Click here to learn more about Adolescent Scoliosis
Adult Scoliosis
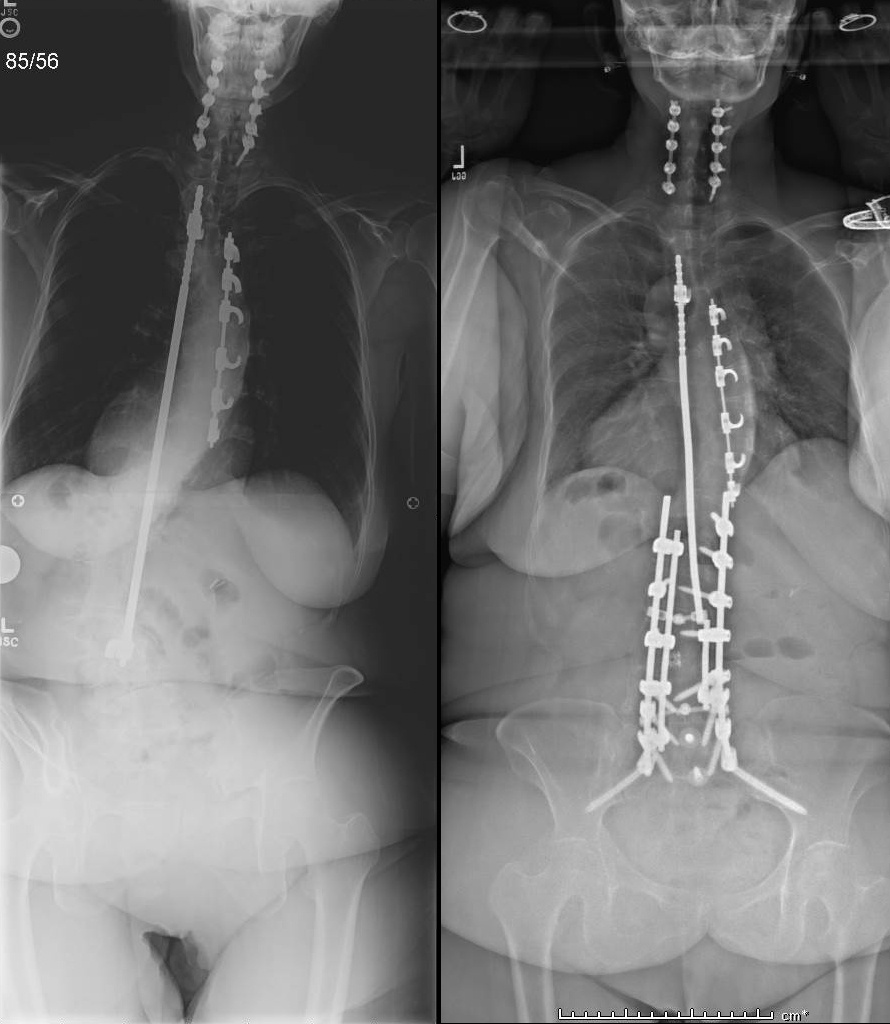
 |
 |
Adult scoliosis can be simply the progression of idiopathic or any other cause of scoliosis causing worsening pain and deformity.
In de-novo degenerative spinal deformity patients often present with loss of lumbar lordosis and mild to moderate sagittal plane imbalance. Coronal plane deformity is typically mild. However, progressive back pain from the degeneration or buttock and leg pains from lumbar spinal stenosis (nerve pinching from bone spurs) may drive a patient to seek treatment.
Patients with pre-existing adolescent idiopathic scoliosis may degenerate either the scoliosis or the spine around the scoliosis because of the normal spinal compressive forces being transmitted through tipped or curved vertebrae and discs. Patients may present with coronal (shifted) or sagittal plane (stooped) deformity. Patients who have developed significant lumbar spinal stenosis (bone spurs pinching nerves) may demonstrate neurologic deficits related to nerve root compression. Or a collapsing spine syndrome may be present with progressive pain and spinal imbalance.
Again, non-operative treatments in adult patients are primary, with osteoporosis treatment, physical therapy and if necessary, injections. If these fail, and either the scoliosis or the disability associated with it progresses, surgery may be necessary.
It is not uncommon in older adults, especially those with lumbar scoliosis, to get accelerated progression and degeneration of their spine below the scoliosis. This can result in a Collapsing Spine Syndrome with progressive back pain, spinal stenosis, and spinal imbalance. Conservative treatments may focus on using bone restorative medicines for treating any existing osteoporosis (such as Forteo/teriparatide), physical therapy when indicated, and injections targeted at the areas of dysfunction.
As a last resort, surgery may be necessary. In these cases, often the most technically difficult given the fragility of the aging spine and aging patient, a range of expertise is necessary. The desire for minimally invasive approaches must be balanced with sound surgical planning.

Marcia - Older Adult Scoliosis
Click here to learn more about Adult Scoliosis
Previously Operated Scoliosis or Spine
Currently, in the high volume centers, spine and scoliosis surgery has a very high success rate using good indications, modern techniques, modern instrumentation, and focused medical management. However, many patients with a previously operated scoliosis or spine may have had an operation with an older technique, had a newly degenerative spine next to the previous operation, or fell in to the small percentage of patients who do not heal. These can be broken down into four general categories.

Flatback Syndrome: Historically, flatback syndrome referred to the use of a Harrington rod being used to treat a lumbar or double scoliosis. In this case, the distractive properties of the Harrington rod led to loss of lumbar lordosis. Patients initially did well, but as they aged, early spine degeneration, along with loss of hip range of motion, led to progressive stooping leading to an accelerated development of disability. Progressive stooping, back pain, and sometimes leg pain from bone spurs can be issues. These problems can form 10-50 years after the initial surgery.
More recently, flatback can occur from lumbar laminectomy or fusion surgery. In these cases the timeline is usually shorter. The other issues in previously operated spines can apply as well, such as non-union, and nerve pinching.
Non-Union: Using current techniques, chance of non union after a scoliosis or spine surgery is relatively low. However, older studies show it to be 10-30%. In these cases, either in the short term or long term, there can be pain, broken rods, progressive deformity, and new nerve pinching.
Nerve pinching/stenosis. In this situation, there is either residual nerve squeezing after the surgery or new nerve squeezing after the adjacent spine has degenerated.
Adding on, junctional syndrome: in any type of scoliosis surgery, the risk of a junctional syndrome is present. In some cases this risk is extremely small (1%) such as in a teenager or young adult with a single right thoracic curve. In other cases this is very high, due to lack of surgeon experience with level selection (Lenke 1AR curves) or difficult curve types (selective fusion in a Lenke 3C curve in a teenager or young adult or a realignment surgery such as a subtraction osteotomy in an osteoporotic patient). This risk can be minimized with the surgical experience, technique, and level choice of the physician and some medical management issues.
In each of the cases above, there are often conservative treatments to try as long as there is evidence for effectiveness and no risk of permanent damage. These include either therapy, bracing, or injections. If these fail, surgery may be necessary. The complexity of revision or repeat surgery necessitates that the surgeon make sure that the spine is aligned, the spine heals properly, and all neural elements are protected and decompressed. Experience in revision surgery, including scar dissection, revision reconstruction, and osteotomy surgery, is important in these patients.
Click here to learn more.
Flatback Syndrome
 When the proper curves in the spine that support an economical stance requiring minimum energy to stand or walk fail, the result is a condition called Flatback syndrome.
When the proper curves in the spine that support an economical stance requiring minimum energy to stand or walk fail, the result is a condition called Flatback syndrome.
Some of the symptoms include having trouble maintaining a proper posture, low back pain and thigh pain. Since the person has trouble maintaining proper alignment, the symptoms might increase throughout the day due to fatigue. Patients might also have upper back and neck pain due to constantly trying to realign themselves. These symptoms can often develop to be very painful and disabling.
Flatback syndrome might be from a previously operated scoliosis. Flatback syndrome was originally used to describe Harrington rods recipients (1960s- early 1990s) due to the fact the rods sometimes flattened the normal sway of the spine. This was due to the rods extending down into the lower part of the spine. The rods were unable to follow the natural curve of the lower back, which caused the spine to unnaturally straighten out. This unnatural movement helped advance the degeneration of discs in the spine.
However, flatback syndrome with severe stooping might be from back ageing, osteoporosis, degenerative disease, lumbar surgery that fails.
No matter the cause, this can manifest as progressive stooping, which can cause severe pain and disablity.
If conservative treatment fails, surgery has dramatic results in standing patients up straight, relieving pain, and improving function.
Click here to learn more about Flatback Syndrome.
 Harrington Rods (first generation scoliosis implants)
Harrington Rods (first generation scoliosis implants)
The Harrington rod was a stainless steel spinal instrument that was implanted in the patient along their spinal column to treat a curvature in their spine starting in the 1960s. Harrington rods were the most common tool used for scoliosis to treat instability and deformity of the spine from 1967 until about 1990.
It is estimated that around one million people had Harrington rods implanted because of scoliosis in its thirty-year history. Newer developments in medicine and medical technology have now made the Harrington rod obsolete. The Harrington rod and its successors are all centered around the same idea that the tools are only designed to temporary correct the curvature in the spine, but it is the actual healing of the spinal fusion which fixes the patient’s condition. These rods have also been widely linked to the development of Flatback Syndrome in recipients.
Click here to learn more.
Scheuermann's Disease in Adolescents and Adults
 Scheuermann's kyphosis, manifesting in a “roundback” or “hunch” deformity, is a developmental type of kyphosis occurring while the body is still growing. Normal vertebrae are rectangular shaped and stacked on top of one another like building blocks with a soft cushion disc between each one. When Scheuermann's kyphosis occurs, the front of the vertebrae wedge forward and closer together in a triangular shape. This causes the spine or curve to move forward and closer together in a triangular shape and the spine to curve forward more than normal.
Scheuermann's kyphosis, manifesting in a “roundback” or “hunch” deformity, is a developmental type of kyphosis occurring while the body is still growing. Normal vertebrae are rectangular shaped and stacked on top of one another like building blocks with a soft cushion disc between each one. When Scheuermann's kyphosis occurs, the front of the vertebrae wedge forward and closer together in a triangular shape. This causes the spine or curve to move forward and closer together in a triangular shape and the spine to curve forward more than normal.
Scheuermann's kyphosis develops in adolescents while their bones are still growing. It happens to about 0.1% percent of people in this age group and occurs a little more often in boys as girls.
This kyphosis, or roundback, can lead in larger curves to difficult spinal deformities and pain. Initial treatments, depending on the age of the patient, residual growth, and size of curve, can include physical therapy, bracing, or injections. In larger or progressive curves resistant to conservative treatment, surgery is an option. This can be done minimally invasively via a dual VATS/percuateous approach, or a single approach Ponte procedure.
In adults in whom Scheuermann's kyphosis is untreated, it can be a cause of progressive roundback, pain, and overall spinal imbalance.
Click here to learn more.