Pediatric and Adolescent Patients
 Given the advances in the field, an experienced surgeon should have very low complications in pediatric and adolescent patient group. However, many surgeries in the past have been performed with older instrumentation techniques such as Harrington rods, Cotrel Dubousset instruments, Luques rods and wires, or other reconstruction techniques.
Given the advances in the field, an experienced surgeon should have very low complications in pediatric and adolescent patient group. However, many surgeries in the past have been performed with older instrumentation techniques such as Harrington rods, Cotrel Dubousset instruments, Luques rods and wires, or other reconstruction techniques.
Judging from multiple academic papers studying pediatric scoliosis surgeries, most surgeons who care for scoliosis patients perform less than 15 scoliosis procedures a year, leading to increased complications and worse patient outcomes than high volume surgeons. This lack of experience can lead to failed surgeries even using current techniques (WORLD NEUROSURGERY, https://doi.org/10.1016/j.wneu.2018.04.103). Other papers show a similar effect with adult scoliosis surgery, where the surgeons less experienced in complex spine had significantly more complications and worse outcomes compared to experienced surgeons (Lee et al. Medicine (2018) 97:34). This is not the case at ScoliosisTexas, where Dr. Geck has 20 years of experience and has performed more than 2500 scoliosis and other spinal deformity surgeries. In addition, we provide our actual quality data in our reporting section.
If a patient has problems after a scoliosis surgery, Dr. Geck has the experience to fix it, whether the issue is non healed fusion, recurrent or progressive deformity, residual inflammation or infection, or issues above or below the rods.
Adult Patients
There are two groups of adult patients who may need revision surgery if they fail conservative treatment.
The first is the patient previously successfully of unsuccessfully treated for scoliosis, usually with Harrington rods, Cotrel Dubousset instruments, or a 3rd generation instrumentation. These patients, despite instrumentation failure, failure of fusion, suboptimal alignment (flatback), often life productive lives, until normal aging sets into their lumbar spine (low back). In these cases, what was a compensated issue can with time turn into a painful flatback in addition to the other issues.
The second is a patient previously treated primarily as an adult for either scoliosis or degenerative spine disease. These patients can get post-laminectomy syndrome, iatrogenic flatback syndrome, adjacent segment disease, non unions, or scar complicating their recovery.
In both of these situations, Dr. Geck has the experience to fix these failed surgeries and restore health related quality of life, reduce pain, and improve function. In these situations, more complicated surgical techniques may be needed.
 Case Study
Case Study
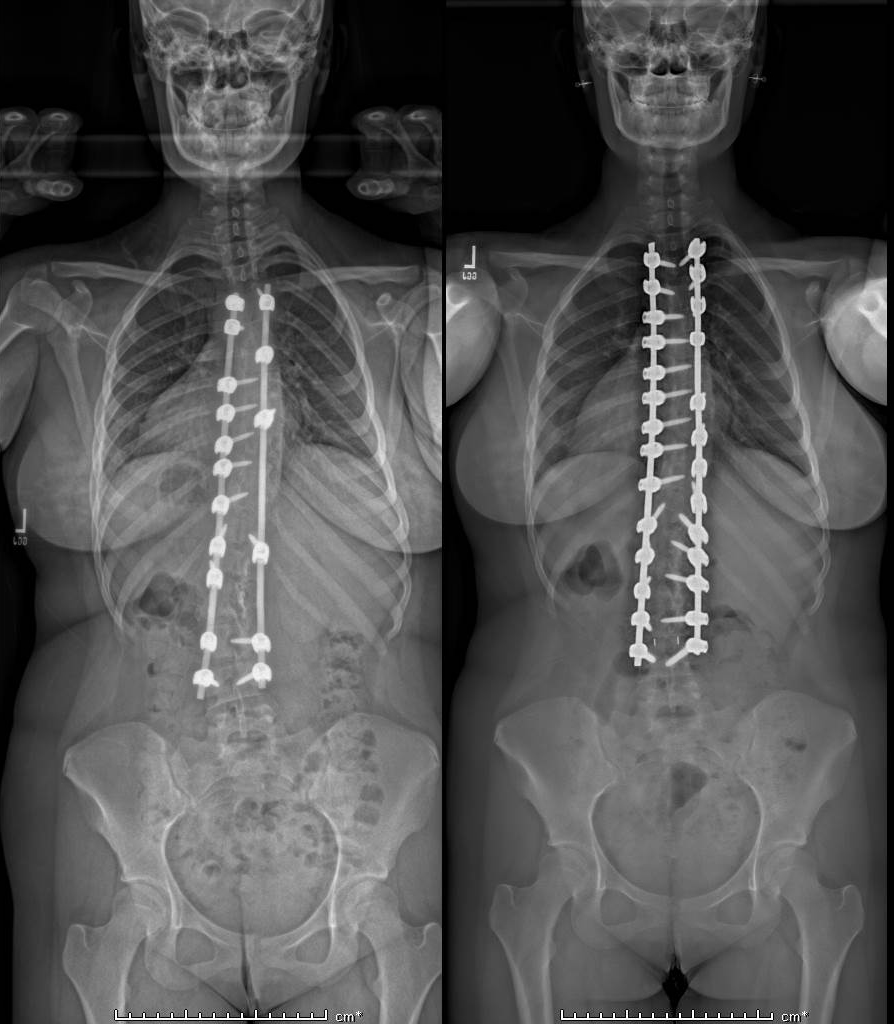
Revision for failed Adolescent Scoliosis Surgery
This 16 year old girl had a previous scoliosis surgery 2 years earlier at another site from T4 to L4. She had significant residual back pain, residually physical and cosmetic deformity, pulled out hardware, and multiple levels of non union (unhealed bony fusion).
She underwent a revision T3-L4 Posterior spinal reconstruction with posterior column osteotomies, revision screw and hardware placement, revision deformity correction, and inter body fusion at L34. 6 months post operatively CT scan showed complete bony fusion. At 12 months, she has no back pain, was back to dance line, with high satisfaction level for her spine appearance.